Extract from The Guardian
Until relatively recently, lethal infectious diseases stalked the lives of Australian children – including my father, Tom Keneally. Vaccines have saved millions.

People queue for immunisation at Maroubra School in July 1939.
Last modified on Sun 15 Aug 2021 16.16 AEST
It’s 1940, and a five-year-old boy lies in an oxygen tent. He struggles for breath and hallucinates that his leaden toy soldiers are alive and marching around the room, monstering him with their bayonets.
He has diphtheria, a disease also known as The Strangling Angel. There is a vaccine, but not every child has been inoculated. The bacterial infection creates a membrane across the back of the throat, cutting off air supply.
The little boy’s mother, sitting a desperate vigil next to the oxygen tent, has seen diphtheria take other children.
It will not, in the end, take her son. The membrane will fail to fully close off his airway, and he will emerge from the oxygen tent. He will attend the funerals of classmates who die of diphtheria and polio. He will, in time, run alongside his friend , a fine athlete born blind after his mother contracted rubella during pregnancy. He will rattle a stone in a can to guide his friend to the finish line.
Throughout his schooling, children he knows will die from disease.

‘I’d like to take anti-vaxxers back in time’, says Tom Keneally, here aged five, shortly before he contracted diphtheria. Photograph: Supplied
He will, through luck, survive. He is still alive now, at the age of 85. He’s my father, and his name is Tom Keneally.
“One of the brothers (the Christian Brothers of St Patrick’s College in Sydney’s Strathfield) would come into the classroom from time to time and tell us someone had died,” Keneally said. “We would say a decade of the Rosary for them, and the brother would say that God takes the best children, and I would be relieved I wasn’t one of those.
“It didn’t feel like an ever-present threat as kids because we were just living our lives, although I think for our parents it was always there, that possibility.”
Some vaccines can also protect against certain cancers later in life. As Prof Raina MacIntyre, head of the Biosecurity Research Program at the Kirby Institute and professor of global biosecurity at the University of NSW points out, the hepatitis B vaccine protects against liver cancer, while human papillomavirus vaccine guards against cervical and penile cancer.
“People don’t remember the gains we’ve made,” McIntyre says.
“In the 19th century, the leading cause of death in children was infectious disease. People would have 10 children and might lose five of them. We lived with high rates of infant mortality,” she says.
As well as two world wars, Australians in the first half of the 20th century had a Spanish flu pandemic and a bubonic plague outbreak to contend with, along with numerous spot-fires of disease.
The
lethal diseases that routinely beset the population – such as the
choking diphtheria, the crippling polio, the wracking tetanus – made
childhood precarious.
Child in an oxygen tent in intensive care. 1950-1959. Photograph: Australian Photographic Agency/State Library of NSW
To modern parents, disease names like polio and smallpox and diphtheria have been relegated by vaccination to arcane words with no practical relevance. But while these cruel diseases no longer kill Australian children, experts say there may be a risk of lapsing into complacency.
“The visibility of the ravages of polio, and the fact that most people knew someone who’d had a child die were really powerful drivers, people were desperate for vaccines,” says David Isaacs, clinical professor in paediatric infectious diseases at the University of Sydney, and author of Defeating the Ministers of Death – The Compelling History of Vaccination. “Many younger people have no concept now of how awful it was.”
Tom Keneally’s diphtheria infection was not to be his last childhood spell in hospital. In 1944 he lay recovering from pneumonia near a boy in an iron lung, suffering from polio. The boy was studying for the Leaving Certificate, the forerunner of the HSC.
“He had a bracket above his head that textbooks could be slid into, and I remember him studying Hamlet,” Keneally says. “His mother was always there, turning pages and changing books, and that’s how he studied.”
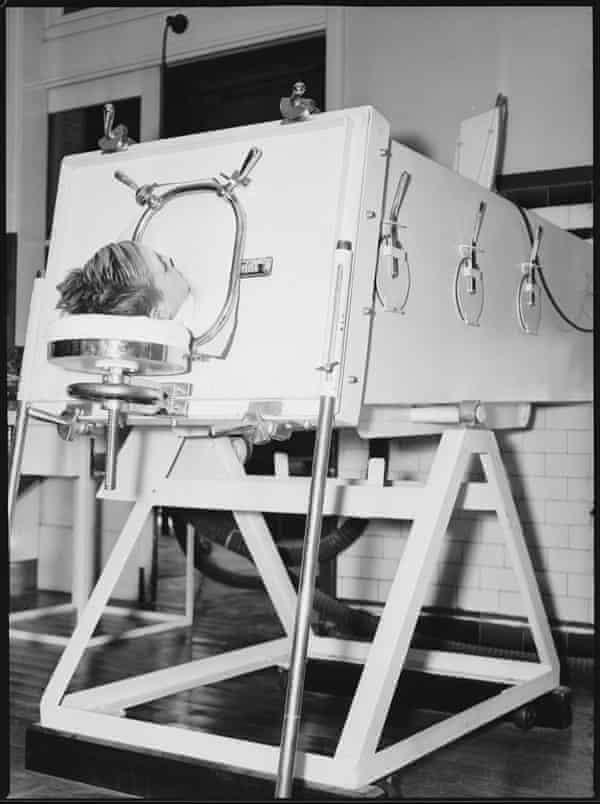
A child lies in an iron lung at the Children’s Hospital 20 May 1938. Photograph: Olson/State Library of NSW
Some time later, he learned the boy had died when a power cut rendered his iron lung useless.
Dr Peter Hobbins, a medical historian at the Australian National Maritime Museum, says polio was still killing children into the 1950s.
“It was a reality of life in Australia. A lot of people don’t realise how many diseases were rampant until relatively recently. There’s a reduced visibility of the consequences of these diseases, people don’t appreciate the fear parents felt of sending a child to school and possibly having them not come back into the family,” he says.
Not that there weren’t triumphs, notably the eradication of smallpox, which Isaacs says killed up to one in three babies in the London of the 18th and early 19th centuries. A campaign by the World Health Organization, starting in 1967, saw it wiped out by 1980.
The first smallpox vaccinations in Australia were given in the early 1800s. That was no good to the people of the Eora nation. In 1789, a disease believed to be smallpox was introduced by the colonists. It tore through the Aboriginal population of Sydney, killing up to 70%.
While smallpox is no longer a threat, MacIntyre warns that diseases we have almost forgotten can easily return if vaccination rates slip.
“One example is the fall of the Soviet Union,” she says. “There were good vaccination programs, and then when the Soviet Union fell, many stopped being conducted.”
As a result, cases of diphtheria, which had been almost unheard of due to vaccination, reached 140,000, and the disease killed 4,000 children and young adults.
“If we stopped vaccinating against diphtheria here, we would see the same,” MacIntyre says.
Despite their life-saving properties, vaccines have often been greeted with suspicion. Hobbins says a tragedy in 1928 had an impact on diphtheria vaccination rates – but it may also have ultimately increased vaccine safety.
“It became known as the Bundaberg Tragedy, or the Serum Tragedy. A batch of diphtheria vaccine contaminated with Staphylococcus aureus was injected in high doses into 20 children, and 12 died,” he says.

Diptheria immunisation, 25 March 1940. Photograph: State Library of NSW
While vaccine mandates are sometimes raised as a counter to vaccine hesitancy, they can backfire. In Defeating the Ministers of Death, Isaacs writes of 80,000-strong protests in the UK city of Leicester in the late 19th century, in response to a smallpox vaccine mandate.
“I truly believe in negotiation and respecting people’s intelligence, because vaccine hesitancy is not about intelligence. A lot of hesitancy is based on fear and misunderstanding, and we don’t want to alienate people,” he says.
“Then you can sometimes bring people around if you’ve developed a close relationship, which is why I’m a firm believer in using GPs to get those messages out.”
Still, Australians are very supportive of childhood immunisation, he says.
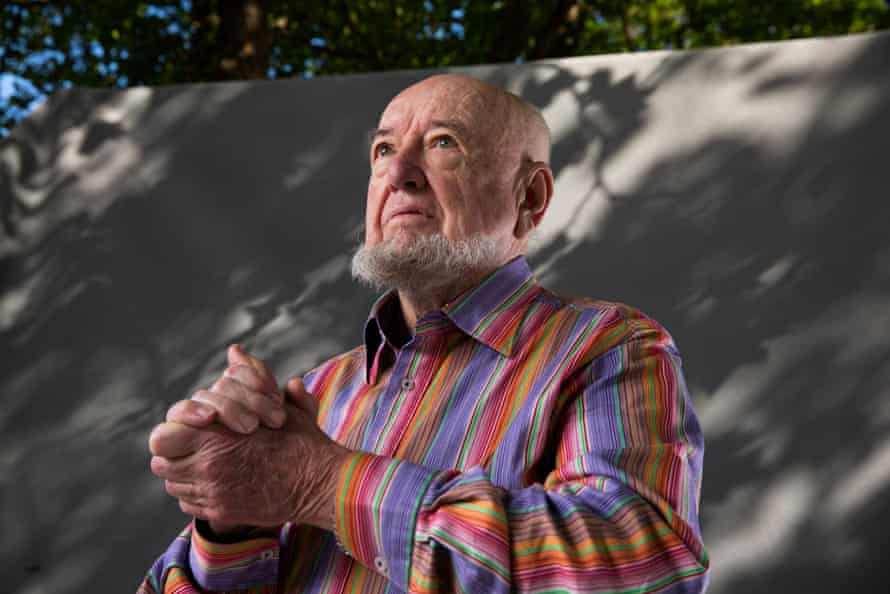
Thomas Keneally, Australian novelist, playwright, and essayist. Photograph: Murdo MacLeod/The Guardian
“Our uptake of routine childhood immunisations is about 95%. That’s enough to give you herd immunity, so that there’s no endemic spread of measles at all.”
MacIntyre agrees.
“Australia has had high rates of vaccination. Anti-vaxxers are around 2%, which is not that much,” she says.
“It’s not so much vaccine hesitancy as vaccine confusion [with Covid-19 vaccines]. I believe we can achieve good rates of vaccination [against Covid-19] in Australia.”
As for committed anti-vaxxers, Tom Keneally knows what he would like to do to try to shift their perspective.
“I’d like to take anti-vaxxers back in time to my childhood. There would be a story on every street which could change their minds.”
No comments:
Post a Comment